
What is vertigo?
Vertigo is a loss of balance that can take several forms and often manifests itself as dizziness, or the false sense that you or your world is spinning. Vertigo is a symptom of underlying balance disorders rather than a specific disease in and of itself.
Symptoms of vertigo:
- Feeling that the room is spinning
- Feeling that you are spinning
- Feeling that the floor is coming up and over your head
- Feeling that you are falling or dropping
- Feeling that your are on a rocking boat
- A general “floating” feeling
- Feeling light-headed
- Motion sickness or sensitivity
- A non-specific history of "balance problems" or being clumsy
Dizziness is one of the most frequent causes of doctor visits, and it can significantly impact your life. It should be noted that dizziness is a symptom that can arise from many different causes, including inner-ear disturbances like vertigo, poor circulation, medications, etc. The nature of the feeling will guide your physician or audiologist in shaping what diagnostic tests and treatment approaches you need, and this article focuses exclusively on vertigo.

According to studies, dizziness (including vertigo) is estimated to affect about 15% to over 20% of adults.
Frequently Asked Questions
This depends on the specific cause of your vertigo, but some common initial signs include:
- Strange sensation of something about to go wrong (aura)
- “Seeing stars” or flashes of light in your visual field
- Feeling light-headed or off-balance
- Sweating
This also depends on the cause. Patients with BPPV may be triggered by specific head movements (looking up, bending down), while those with Meniere’s may be triggered by dietary changes such as drinking caffeine or eating salty foods. Vertigo is a very individualized disorder. As such, it’s helpful to keep a log with the following information to help you and your healthcare team better understand your vertigo:
- Any medications you take and what time of the day you take them
- Time of day of the attacks
- Duration of the attacks
- Nature of the vertigo (spinning, dropping, swaying, etc.)
- What you were doing just before the attack
- Other symptoms such as ringing in the ears (tinnitus), nausea, sweating, vomiting
- What you can do to make it better such as lying down, turning off the lights, sitting on a hard-backed chair
- What makes the vertigo worse?
For some disorders like BPPV, yes, vertigo can be treated and will essentially go away. Other types of vertigo are part of chronic disorders. The key to living well with vertigo is to understand it and have a solid safety plan so that if and when an attack comes, you are prepared. Working with your diagnostic and treatment team—particularly a physical therapist—can be very helpful in creating and maintaining this plan.
On the psychological side, it’s important to get peer support for chronic vertigo. The Vestibular Disorders Association website can connect you to local and remote support groups. With the support of these folks, as well as an ongoing relationship with your healthcare team, living with vertigo is possible and doesn’t need to be scary or dangerous.
How normal balance function works
Human balance is a carefully coordinated interaction between three systems:
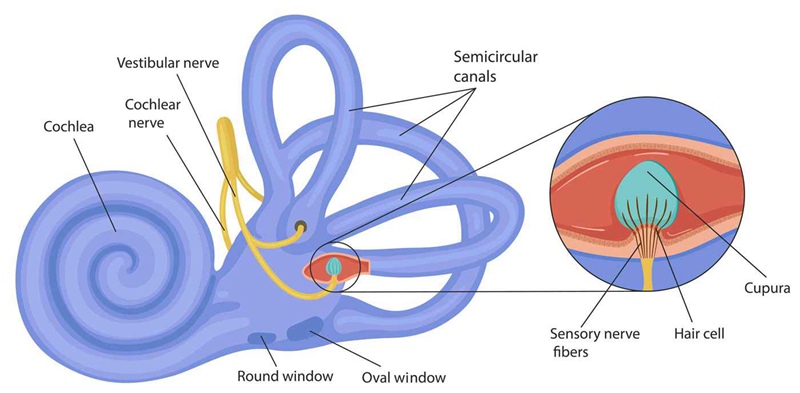
- The inner ear, part of which consists of the left and right labyrinths—which are the inner ear organs responsible for your sense of balance,
- Eye movement mechanisms, and
- Our body awareness system (called proprioception or kinesthesia) which matches movement, motion, and bodily location.
Information from these input systems is coordinated in the brainstem. Consider the following common example:
You’re sitting at the kitchen table browsing articles on HearingTracker as you enjoy your morning coffee. Your brain knows you’re sitting still because the fluid and crystals (otoconia) in your labyrinthine structures are still and your proprioceptive system is reporting that about 80% of your weight is on your keister and 10% on each foot. You hear some noise outside your window and turn your head to check it out.
At that point, your brain gets a report of a 90-degree positive response from your right labyrinth, and an equal and opposite response from the left labyrinth. Your eyes move 90 degrees to the left to prevent a visual “whoosh,” and your proprioceptive system reports that the “tuchus-footus” ratio is unchanged. All this means that the only possible option is that you must have moved your head 90 degrees to the right while your body remained still.
Using this basic understanding of how things should work, let’s look at some common causes of vertigo.
Common Treatments for Vertigo and Dizziness
There are a number of treatments for vertigo, including physician-led strategies as well as some that are more self-directed.
Traditional Treatments
After your vertigo is diagnosed, you may be referred to a specially-trained physical therapist for vestibular rehabilitation. This generally includes functional tests to better identify exactly which parts of the balance system are weak or misbehaving, and then a customized set of exercises to improve the function of those weak components.
It’s common to have a few sessions a week with the therapist in addition to daily at-home practice. Generally, vestibular rehab will last for 6 to 12 weeks with several re-checks of function and strength along the way. In most cases, if the referral comes from your primary care provider, these costs of vestibular rehab are covered at least partially by insurance.
For acute symptoms, your physician may prescribe an anti-vertigo medication like Meclizine which essentially “turns off” the signals coming from the affected inner ear. It’s very important to take this as prescribed, because this and other anti-vertigo drugs may have side effects including drowsiness which make it difficult to get around. Another danger of over-using medication designed for acute symptom care is that your brain becomes accustomed to it, making it less effective when you actually need it. Finally using these drugs chronically can interfere with your body’s ability to compensate to the vertigo.
How to Ease Symptoms at Home
If you don’t have access to formal vestibular rehab, you can improve your balance using a few simple tips and tricks.
- Make sure your general health is on point. Schedule a physical and make sure that your cholesterol, blood pressure, and blood glucose (sugar) levels are well controlled and that any medications you are taking are well managed.
- Review the reports of any vestibular testing to see if they included at-home exercises.
- Visit the Vestibular Disorders Association website. This great resource includes links to professionals familiar with vestibular disorders as well as an entire section on at-home exercises.







